What is rectal prolapse?
Rectal Prolapse is a condition in which the rectum ( i.e. the last few inches of the large intestine ) or a part of it, loses its normal attachments inside the body, and protrudes out through the anal opening. Although it is never an emergency problem, it does leave the patient uncomfortable and anxious, with a significant negative impact on the quality of life.
CAUSES OF RECTAL PROLAPSE?
- Long standing constipation with history of straining to defecate.
- Chronic diarrhoea
- Old age – Due to laxity of the pelvic floor muscle and reduced anal sphincter tone.
- Pregnancy, difficult vaginal delivery, multiple vaginal deliveries.
- Chronic cough due to COPD or any other cause
- Neurological conditions like multiple sclerosis, injury to the lower back or pelvis, spinal tumours.
- Cystic fibrosis in children
SYMPTOMS OF RECTAL PROLAPSE?
- The most common symptom is something lump/ swelling coming out of the anal opening. In the early stages, this may happen only during a bowel movement, but as the condition progresses it may happen on coughing, sneezing and standing up as well.
Initially it may be possible to push back the swelling inside with your fingers. With time, even this may not be possible and it may persistently stay out. - In case of Occult prolapse there is no swelling coming out but there may be a sense of incomplete evacuation after a bowel movement, as though something is still left in the rectum.
- Fecal incontinence leading to soiling of clothes. There may be leaking of gas, liquid/solid stools or mucus/ blood stained discharge. The anal sphincter is made of muscles that allow one to hold on to their stool when there is an urge to defecate. When the rectum prolapses, it goes past the anal sphincter, and this allows stools and mucus to pass in an uncontrolled fashion.
TYPES OF RECTAL PROLAPSE!
- PARTIAL OR MUCOSAL PROLAPSE
Only the inner lining of the rectum protrudes through the anus. It is usually <2cm and produces radial folds. - FULL THICKNESS RECTAL PROLAPSE / PROCIDENTIA
Part of the wall ( including all three layers ) protrudes through the anus. It is about 2-5cm and produces concentric rings. - OCCULT or INTERNAL INTUSSUSCEPTION
The rectum folds on itself but does not protrude through the anus.
Treatment of rectal prolapse
- Abdominal approach – Through the belly.
- Perineal approach – Through the bottom.
THIERSCH PROCEDURE:
The best course of action for treating an obstetric fistula is surgery to close it. Most women see a significant improvement in their quality of life following a successful fistula repair. Women can resume their regular lives, engage with friends and family without restriction, and have happy marriages.
Simple vaginal surgery can treat 80% to 90% of patients with vesico-vaginal fistulas. It could take several tries to achieve continence with more complex fistulas.
Being a proctology clinic, Lazocure specializes in the treatment of recto-vaginal fistulas. The fistula is patched up layer by layer. The initial reconstruction is completed. The sphincter has been fixed. Repairing the vaginal wall comes next. The rectal mucosa is finally restored.
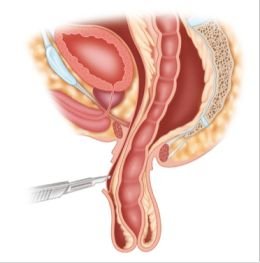
RECTOPEXY ( Abdominal/ Laparoscopic ):
During this process, the pelvic floor and the loose rectal attachments are separated from the pelvic walls. The rectum is subsequently dragged upwards and fastened in a variety of ways to the sacrum, or rear wall of the pelvis, during a procedure known as a rectopexy. Sometimes a segment of the colon is removed in conjunction with this treatment.
Rectopexy resolves the issue, although the function (constipation or incontinence) might not always get better. Conversely, 15% of individuals experience constipation following surgery for the first time. About half of the patients experience worsening of their pre-surgery constipation.
A major surgery performed under general anesthesia is a rectopexy. The patient is prohibited from oral intake for a maximum of three to four



